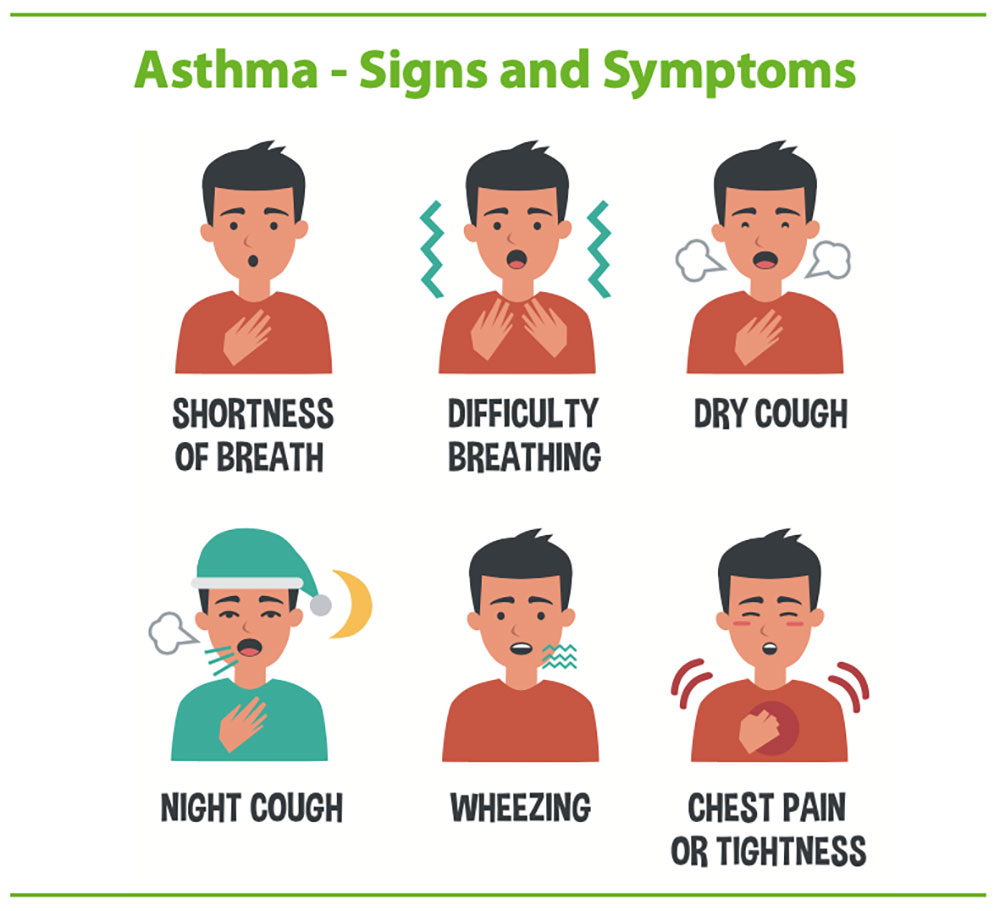
Asthma is a chronic, reversible disease of the airway that is characterized by inflammation and hyperreactivity, resulting in breathing difficulty. Asthma affects 5-10% of the population in the United States and is very common among children.¹ A diagnosis of asthma is based on patient symptoms, physical exam findings, and diagnostic tests such as spirometry and chest x-rays. Blood tests are not necessary to diagnose asthma. Symptoms of asthma include coughing (usually worse at night), wheezing, chest tightness, and breathing difficulty. Your medical provider will also look for signs of respiratory distress, runny nose, nasal polyps/swollen turbinate, and skin eczema.
- While asthma is not preventable, you can control it by taking the following steps: ²
- Educate yourself about asthma and how to control it.
- Obtain allergy shots¹
- Treat related conditions, such as allergies, eczema, sinusitis, acid reflux, sleep apnea, obesity, stress, and depression
- Use a peak flow meter – handheld device that indicates how well you are able to move air into and out of the lungs³
- Take your asthma medications as prescribed.
- Identify and avoid asthma triggers
- Animal dander, dust mites, cockroaches, indoor/outdoor mold, pollen, tobacco smoke, smoke, strong odors, and sprays
- Vacuum cleaning
- Sulfites in foods and beverages
- Cold air
- Other medications² ⁴
- Stay physically active.² Talk with your healthcare provider about how to safely incorporate exercise into your daily life.
- Monitor and log your asthma symptoms and level of control. Asthma is well-controlled if:³
- Symptoms are present no greater than 2 days/week, and do not wake you more than 1-2 nights/month
- You are able to perform all of your normal activities
- You use quick-relief medications no more than 2 days/week
- You have no more than one asthma attack per year that necessitates use of inhaled corticosteroids
- Peak flow results do not dip below 80% of your personal best
- Visit your health care provider for regular a checkups.
What are the risk factors for asthma?
Common risk factors for asthma are genetics, gender, race, body mass index (BMI), viral infections, animal and airborne allergens, tobacco smoke, exercise, obesity, emotional stress, non-steroidal anti-inflammatory drugs (NSAID) (aspirin, ibuprofen, Aleve, naproxen), β-blockers (prescription medications, such as atenolol, metoprolol, labetalol), and food allergies.¹
How is asthma treated?
The treatment of asthma depends primarily on its level of severity.¹ General measures include identification and avoidance of exposure to triggers and use of prescribed medications, such as rescue inhalers, corticosteroid inhalers, leukotriene inhibitors, and EpiPen’s. All patients benefit greatly by using “spacers” with their inhalers because spacers more readily direct inhaled agents into the lungs.¹ Spacers are holding devices that attach to inhaler devices to enable effective delivery of medication to the lungs.⁵ Using an inhaler without a spacer often leads to ineffective use of the inhaler because the medication stays in the mouth rather than being inhaled into the lungs prior to exhalation. Patients with severe or poorly controlled asthma, with comorbidities, and/or children with moderate to severe persistent asthma should be referred to an allergist or pulmonologist.
What other healthy lifestyle habits are recommended for people with asthma?
In addition to the previously discussed behaviors, individuals with asthma should maintain an active lifestyle by exercising on a regular basis (only after their health care provider provides medical clearance).⁶ Exercise can benefit people with asthma by reducing the ventilatory effort required for a variety of tasks. Oftentimes, people with asthma require medications, such as inhalers, anti-inflammatories, and steroids to prevent exercise-induced or exacerbation of asthma. In most cases, people with controlled asthma can follow similar exercise guidelines as the general population.
What, if any exercises, are best for people with asthma?
Exercises, such as walking, cycling, and swimming are best for people with asthma.⁶ Yoga can also benefit people with asthma because it targets deep breathing, which helps to cleanse the body of carbon monoxide thereby increasing the blood’s ability to carry more oxygen, improve circulation, and promote energy.⁷
Are there any exercises that people with asthma should avoid?
Upper body exercises, such as cross-country skiing, rowing, and arm cranking require higher ventilation demands and may not be appropriate for some people with asthma.⁶
Exercise tips for individuals with exercise-induced asthma:⁶
- Always receive medical clearance from your primary care provider before starting to exercise.
- Always carry your rescue inhaler with you during exercise.
- Use your rescue inhaler before exercising if prescribed and recommended by your healthcare provider.
- Avoid becoming dehydrated by drinking plenty of fluids before, during and after exercise.
- Avoid asthma triggers when exercising.
- Exercise indoors during temperature extremes or when pollution/pollen counts are high.
- Warm up and cool down gradually and over a prolonged period of time.
- Start exercising at a low intensity with gradual increases. If symptoms of asthma start to develop, reduce intensity.
- Exercise in mid-to-late morning hours.
- Individuals with stable, well-controlled asthma are generally able to follow general exercise guidelines for cardiovascular and strengthening exercises.
- Use your asthma medications as prescribed.³
- Call your health care provider if your asthma symptoms persist despite the proper use of your medications and Asthma Action Plan.
©2023HealthSpot References: (1) 5MinuteConsult. (2016). Asthma. Retrieved from http://5minuteconsult.com/collectioncontent/1-151423/diseases-and-conditions/asthma (2) National Heart, Lung and Blood Institute. (2014). How can asthma be prevented? Retrieved from https://www.nhlbi.nih.gov/health/health-topics/topics/asthma/prevention (3) National Heart, Lung, and Blood Institute. (2014). How is asthma treated and controlled? Retrieved from https://www.nhlbi.nih.gov/health/health-topics/topics/asthma/treatment (4) Food and Drug Administration. (2017). Food and Drugs [Code of Federal Regulations, Title 21]. Retrieved from https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfCFR/CFRSearch.cfm?fr=201.22y (5) American Academy of Allergy, Asthma, and Immunology. (2017). Spacers with inhalers: Do they make a difference? Retrieved from https://www.aaaai.org/global/latest-research-summaries/New-Research-from-JACI-In-Practice/spacer-inhaler (6)American Council on Exercise. (2014). American Council on Exercise Personal Trainer Manual (5th ed.). American Council on Exercise: San Diego, CA (7) Waller, P. (2010). Holistic Anatomy: An Integrative Guide to the Human Body. North Atlantic Books: Berkeley, CA

